What is it and why is it important in practice?
During a round of consults, a client bought in a young puppy who was worryingly flat. I quickly swept him out back and started to do all that I could think of to help stabilise this patient. I knew I was forgetting something obvious but I could not figure it out. As I was starting the patient on fluids I heard one of the nurses quietly turn to the other and whisper, ‘I bet he’s hypoglycaemic.’
It was the obvious thing that I had forgotten. I immediately grabbed the glucometer and, sure enough, he was. We corrected the deficit and the patient made a full recovery. If you’re interested, we suspected it was an extreme post-vaccine reaction that had made the little one not eat for a while.
As the patient was improving, I accosted this nurse. I accused her of knowing that I had missed something and not saying anything. From my perspective, she had put the animal at risk with her omission. She looked at me over the patient and calmly replied that she was scared of being told off for giving suggestions. I scoffed at this, who would possibly do that? She replied that one of the other vets had done just that yesterday.
Here was a woman who did not feel psychologically safe at work.
It was not my finest hour of interacting with another member of staff but it really opened my eyes. The practice had undercurrents of tension that I struggled to recognise and name. This manifested as staff not feeling able to speak up, constantly checking every step with someone more senior and generally low morale.
Working in the soup I struggled to understand it. That was until I heard the phrase, psychological safety. It felt like the answer.
What is psychological safety in the veterinary workplace?
Psychological safety at work concerns whether a worker feels safe and accepted in their environment. The psychological aspect refers to a feeling of safety in tasks and interactions with clients and staff. This is of course a separate issue to physical safety that involves muzzling dogs that see you as the enemy or radiation protection (although if you don’t feel protected in that way you will not feel psychologically safe).
Staff that feel safe at work will show up as empowered members of the team. They are able to ask questions confidently, speak up when they disagree with something without fear of retribution and make suggestions without fear of ridicule. Importantly for vet practices, they feel that they are able to share when they have made a mistake, allowing for prompt correction if needed. They will trust and follow the protocols that have been put in place to allow enhanced patient safety and clinical standards.
I think that there is an extra definition for veterinary staff, psychological safety also encompasses a feeling of protection when practicing. Each member feels that there is a safety net when practicing medicine which can have variable outcomes even when the textbook has been followed by the letter. This can be in the form of confidence that they are working to a high standard where easy mistakes are caught/prevented by daily protocols. They also know that there is protection in the event of a complaint or unforeseen negative patient outcome that could occur despite the processes in place. Management will have their back.
Why is it important for vet practices?
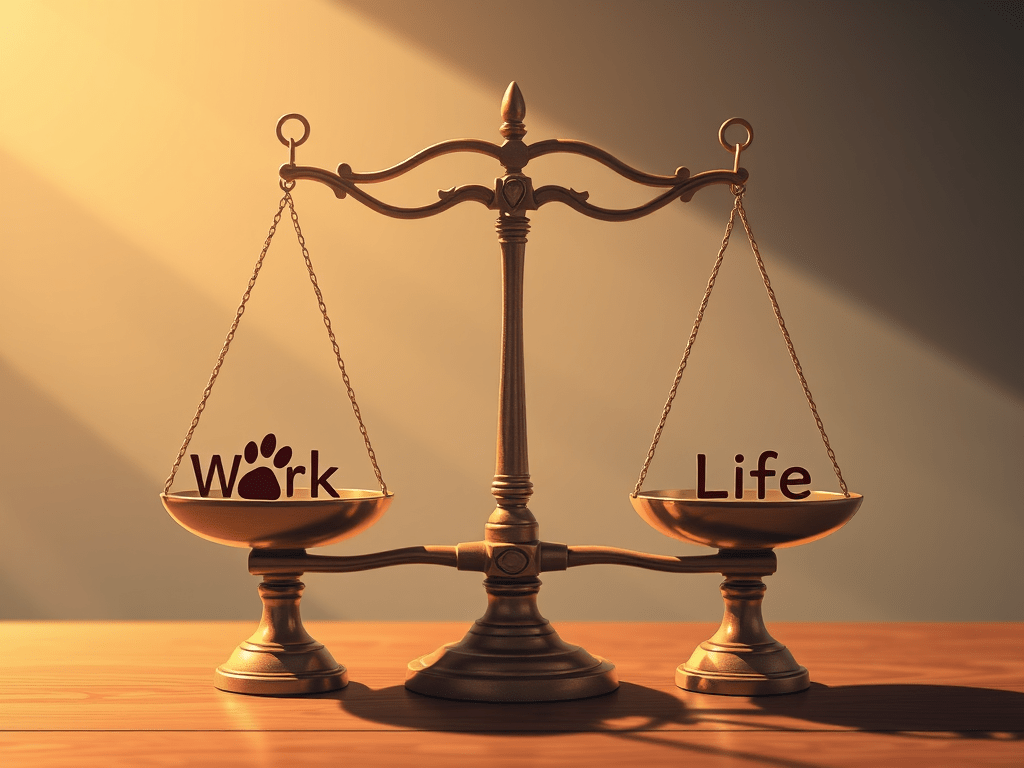
- Improved staff satisfaction, reducing burnout and staff turnover.
- A practice can run with gaps in psychological safety. I have worked in those practices, but morale will never be what it could be. When people feel empowered to do their jobs they will be happier doing them and less likely to leave which is always disrupting.
- Feeling empowered will reduce the chronic stress associated with work and therefore reduce the risk of burnout.
- Improved Patient Safety.
- Following processes such as surgical checklists or admission protocols can help make sure nothing is forgotten when someone is slightly off their game first thing in the morning. The pressure of keeping everything in your head can be reduced and trainees can get up to speed quicker. This immediately benefits the patients and their safety. Not only will calmer staff do better and kinder work, patients will be less likely to have things missed.
- Improved trust from leadership
- When a culture of kind words and instant feedback are present, leadership can trust their team more. Leaders can trust that issues and mistakes will be raised freely and so don’t need to micromanage each person. The ability to delegate will hopefully allow them to spend a bit more time fostering a psychologically safe environment. This will feed into a cycle of staff also trusting their leaders, enhancing psychological safety further.
How can anyone help foster it?
A lot of psychological safety lies with leadership. It can be very hard to make meaningful changes without a push from managers. Specifically putting protocols in place can be hard to implement when you have no control yourself. You do however have power in what you do each day and in how to interact with your team. You do not need to be in a position of leadership to help your team feel respected and accepted by you.
As someone who is not a leader, I feel unable to speak to the larger points. Here are a few small things I think can really help you take responsibility for your part in making others feel psychologically safe. It can also help your own feeling of safety by fostering habits and interactions that will help enhance your practice. The perfect work place doesn’t exist so you can try to enhance your experience wherever you are.
- Be aware of your words.
- Try to be kind and open with staff. Invite opinions and try not to take different options badly. Of course, do everything you can to avoid outbursts.
- Give criticism if invited in a delicate manner and be open to your own. Be very careful here as we are sensitive to criticism. It can be hard when you take pride in your work to receive it but if you can demonstrate taking it with grace then hopefully others will do the same.
- Do not gossip or spread rumours. I know it can be fun and an easy form of bonding but it really only enhances separation in the team. People will notice and eventually not trust you with things they feel vulnerable about. This will lead to them not feeling safe with you.
- Try to debrief when something bad has happened. If the practice does not have those kinds of regular meetings you can have your own low key one with the other members affected so that you can discuss ways to prevent it from happening again. Try to pick an appropriate time though, just venting during a surgery is not the right moment.
- Check in with your team appropriately
- Discuss cases and invite opinions from your team. Get people used to discussing their clinical opinions with you. Allow everyone to feel able to question you (within reason), you never know who will pipe up and remind you of something important.
- Have your own checklists for processes that stress you
- For example, I have a personal pre-surgery checklist for each patient. This way I am satisfied that I haven’t missed something obvious. I’ve put a simplified version of it below:
- Read clinical history
- Examine patient
- Check consent form and populate GA form with any extras from the nurse admit
- For example, I have a personal pre-surgery checklist for each patient. This way I am satisfied that I haven’t missed something obvious. I’ve put a simplified version of it below:
So, I hope my brief introduction to the subject is helpful. Even just putting a name to the tension I had felt in practice has really helped me to understand it. I hope it will help me reduce any negative impact I inadvertently put on my team.



Leave a comment